SUSTAINED-RELEASE PRODUCT CANDIDATE TO TREAT EPISODIC DRY EYE
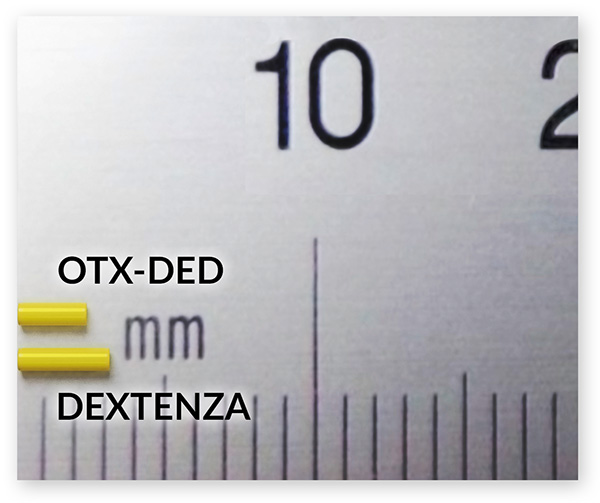
Our newest product candidate, OTX-DED, is a low dose, intracanalicular insert of dexamethasone for the treatment of patients with episodic dry eye disease. OTX-DED is designed to release dexamethasone over a period of two to three weeks for the short-term treatment of the signs and symptoms of dry eye disease.1
Many dry eye patients experience exacerbations of their signs and symptoms likely related to inflammation.3 Currently available topical ophthalmic steroids have preservatives4-8 which can result in ocular surface toxicity.9 These drops may also lead to adverse events such as elevated IOP or increased risk of infection if used chronically.10 OTX-DED may offer these patients the opportunity to be treated with a physician-administered, preservative-free and hands-free steroid therapy.1
EXISTING TREATMENTS
- Slow onset of action3,11
- Burning/stinging upon application11,12
- Topical ophthalmic steroids can be misused13
- Contain preservatives4-8 which may cause ocular toxicity9
PRODUCT CANDIDATE ATTRIBUTES1
- Dexamethasone loaded in hydrogel
- Preservative-free
- Occludes the punctum
- Fully biodegradable insert
Caution: OTX-DED is currently undergoing clinical evaluation and is limited by law to investigational use only. This product has not been approved by the FDA as safe or effective.
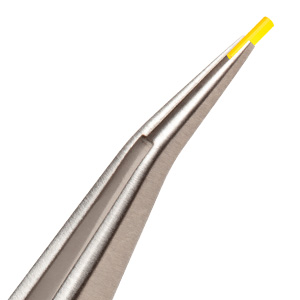
Intracanalicular insertion of OTX-DED
About Episodic Dry Eye3
Most patients with chronic dry eye disease experience episodic flares which can last from a few days to a few weeks. Flares may be triggered by various environmental stresses including allergies, dry indoor heating or cooling, smoke, contact lenses, or medications. Flares are typically associated with rapid worsening of eye discomfort followed by prolonged, increased inflammation. During an acute flare, eye surface inflammation is initiated by a nonspecific innate immune response. This may be followed by a slower, more specific adaptive immune response in some patients.